Enteral vs. Parenteral Feeding & Nutrition: A Complete Guide

Verified by Kiera Powell, R.N. and written by Chad Birt on Wed Feb 02 2022.
Medically Verified
Many chronic health problems require special dietary needs, like enteral or parenteral feeding. If your loved one is unable to swallow or digest food normally, these nutritional regimens may be necessary. But what’s the difference between enteral and parenteral feeding? And how can you ensure you’re providing the best possible care?
To assist you on your journey, we’ve developed a comprehensive guide to enteral vs. parenteral feeding and nutrition.
What’s the difference between enteral and parenteral feeding?
While the terms "enteral" and "parenteral" sound similar, they represent distinct approaches to providing nutrition.
What is enteral feeding?
Enteral feeding delivers liquid nutrition directly to the gastrointestinal (GI) tract. Individuals receiving enteral feeding consume their meals through a feeding tube, which connects to their stomach or small intestine. This method uses the body's natural digestive pathways. Enteral feeding can provide supplemental nutrition or account for a patient's entire caloric intake.
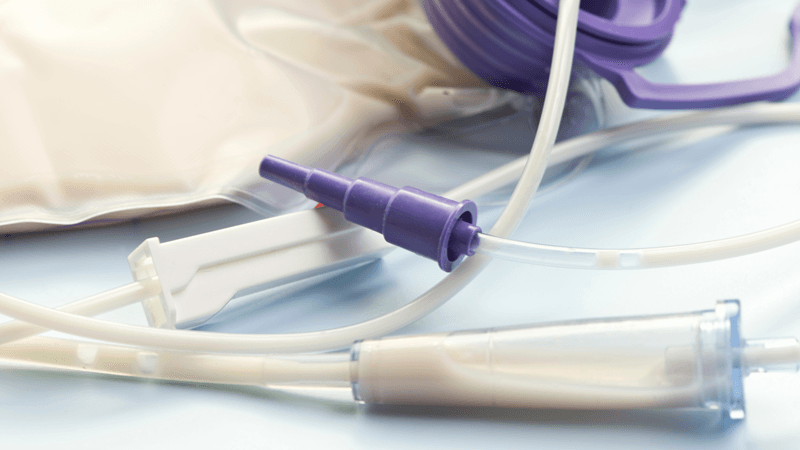
What is parenteral feeding?
Parenteral feeding bypasses the digestive system entirely, delivering liquid nutrition directly into the bloodstream through a vein. It's often considered riskier than enteral feeding due to the direct access to the bloodstream but can lead to significant improvements in health and energy when the GI tract isn't functional. Some individuals use parenteral feeding for short-term recovery (e.g., after surgery), while others require it long-term.
Why would someone need enteral vs. parenteral nutrition?
There are several reasons someone might need enteral or parenteral nutrition:
Enteral nutrition
Enteral nutrition reduces the risk of malnourishment, or a lack of vitamins, minerals, and nutrients. If your loved one isn’t able to eat enough calories throughout the day, they’re more likely to lose weight and experience serious health problems.
Common conditions that may benefit from enteral feeding include:
Stroke (causing swallowing difficulties)
Certain Cancers (especially those affecting the head, neck, or esophagus)
Dysphagia (difficulty swallowing)
Neurologic or Movement Disorders (e.g., Parkinson's disease, advanced Alzheimer's disease)
Critical Injuries (e.g., severe burns, trauma)
Need enteral feeding formulas? Explore our wide selection of enteral feeding formulas designed to meet various nutritional needs. If you need personalized guidance, speak with one of our friendly Customer Care Specialists by calling (800) 696-2273.
Parenteral nutrition
Parenteral nutrition is like enteral nutrition in that it helps prevent malnourishment. However, it’s designed to assist individuals who have gastrointestinal issues that prevent them from properly digesting food. Parenteral feeding administers sugar, carbohydrates, proteins, lipids, and other nutrients through a needle and into a vein. These nutrients ensure your loved one receives the energy and hydration they need to thrive.
Common conditions that may benefit from parenteral nutrition include:
Crohn's Disease (severe cases or flares)
Certain Cancers (with severe digestive complications)
Short Bowel Syndrome
Ischemic Bowel Disease (low blood flow to the bowels)
Severe Pancreatitis
Intestinal Obstruction
What are the types of enteral vs parenteral feeding?
A healthcare provider, often in consultation with a nutritionist, will recommend the specific type of feeding based on your loved one’s age, overall health, medical history, and nutritional needs.
Types of enteral feeding tubes
Enteral feeding tubes are categorized by where they enter the body and where they end in the GI tract. The six main types include:
Nasogastric Tube (NGT): Inserted through a nostril and into the stomach
Orogastric Tube (OGT): Inserted through the mouth and into the stomach (often used in infants or for short-term feeding).
Nasoenteric Tube: Inserted through a nostril and into the intestines.
Nasojejunal (NJ) Tube: Ends in the jejunum (middle part of the small intestine).
Nasoduodenal (ND) Tube: Ends in the duodenum (first part of the small intestine).
Oroenteric Tube: Inserted through the mouth and into the intestines.
Gastrostomy Tube (G-Tube): Surgically inserted through a small incision in the abdomen, directly into the stomach. These are often used for longer-term feeding.
Jejunostomy Tube (J-Tube): Surgically inserted through a small incision in the abdomen, directly into the jejunum, a part of the small intestine. Also used for longer-term feeding, particularly if stomach feeding isn't tolerated.
Looking for tube feeding supplies? Shop our comprehensive selection of enteral feeding medical supplies. For more in-depth information, read our detailed guide on enteral feeding.
Types of parenteral feeding
As previously mentioned, parenteral feeding is designed for people with gastrointestinal or digestive issues. There are two main types of parenteral feeding, including:
Total Parenteral Nutrition (TPN):
Purpose: Used for long-term nutritional needs or when a person requires complete nutritional support bypassing the gut.
Administration: Requires a central venous catheter (CVC) or a peripherally inserted central catheter (PICC line) inserted into a large vein (like the superior vena cava) that goes directly to the heart. This often involves a brief outpatient procedure.
Equipment: A needleless access port may be used to simplify the feeding process.
Peripheral Parenteral Nutrition (PPN):
Purpose: Typically used for short-term nutritional needs (e.g., while recovering from an operation) when less concentrated nutrition is required.
Administration: Administered through a traditional intravenous (IV) line placed in a smaller peripheral vein (usually in the arm).
Do enteral or parenteral nutrition present risks?
Both enteral and parenteral nutrition are generally considered safe and can be well-tolerated, but it's important to be aware of potential risks and side effects.
Potential side effects of enteral nutrition include:
Aspiration: Food getting into the lungs (a serious risk).
Infection: At the tube insertion site.
Gastrointestinal Issues: Nausea, vomiting, diarrhea, constipation.
Skin Irritation: Around the tube site.
Tube Complications: Blockage, dislodgement.
GI Discomfort: If transitioning back to solid foods after long-term enteral nutrition.
If your loved one only needs enteral nutrition for a short time, they might also experience gastrointestinal discomfort as they readjust to solid foods.
Potential side effects of parenteral nutrition include:
Catheter-Related Infections: Due to direct access to the bloodstream, these can be serious.
Blood Clots: Can form around the catheter site.
Metabolic Complications: Liver disease, bone disease, electrolyte imbalances.
Nutrient Imbalances: Can lead to symptoms like fatigue, memory loss, or increased urination
To reduce the risk of these issues, strict adherence to hygiene protocols is crucial. This includes regular cleaning and sterilization of all feeding components (tubes, catheters, needleless access ports, syringes. Explore our assortment of enteral feeding supplies here. Always speak with your loved one’s primary care physician or nursing team if you have any questions about proper hygiene or sanitation.
What is the outlook for someone using enteral vs. parenteral feeding?
Both enteral feeding and parenteral feeding require significant lifestyle changes. It’s normal to feel stressed out or overwhelmed, especially during the first few days or weeks. If you have questions or concerns at any point, contact your loved one’s doctor, nutritionist, or home health providers. They can correct any mistakes, provide key insights, and help you establish a feeding routine.
After making the switch to enteral or parenteral nutrition, your loved one will experience enhanced energy and improved health. At each subsequent check-up, their doctor will run tests and reevaluate their nutritional needs, making adjustments to the treatment plan as necessary.
Frequently asked questions: Enteral vs. parenteral nutrition
Why is enteral feeding preferred over parenteral feeding?
Medical providers generally prefer enteral feeding because it's less costly, less invasive, and presents fewer complications. Additionally, enteral feeding utilizes the body's natural digestive processes, encouraging more efficient nutrient absorption and stimulating intestinal blood flow, which supports the body's natural healing process.
What is the difference between enteral and parenteral routes of administration?
Enteral nutrition is administered directly into the stomach or intestines via a feeding tube.
Parenteral nutrition is administered directly into a vein through an intravenous (IV) line, bypassing the digestive system. This can be a peripheral IV in the arm (for PPN) or a central IV surgically placed into a larger vein (for TPN).
Why is enteral a better choice over parenteral nutrition?
Enteral nutrition isn't necessarily "better" in all cases, but it is generally preferred when feasible. It's less invasive and delivers nutrients directly to the gastrointestinal tract, which is the body's natural route for digestion and absorption. For people recovering from an illness or injury, it offers a safe and effective way to maintain energy and promote healing. Furthermore, feeding tubes are often simpler to manage, clean, and sterilize compared to IVs or central lines, which carry a higher risk of serious infection.
What is the difference between TPN and PPN?
Total Parenteral Nutrition (TPN): Prescribed for long-term nutritional needs or when the digestive system is severely damaged or non-functional. TPN requires a central vascular access device (like a PICC line or CVC) inserted into a large vein leading to the heart.
Peripheral Parenteral Nutrition (PPN): Less invasive and recommended for people with temporary or less severe nutritional needs. PPN is administered via a traditional IV placed in a smaller, peripheral vein, usually in the arm.
Other Articles You May Like

Enteral Feeding at Home
Caring for a loved one who’s unable to chew or swallow their food often requires enteral feeding at home. While administering meals and snacks through a feeding tube might seem daunting, with patience and practice, it’s possible, even if you don’t have a medical background.
Read More >
Common PEG Tube Problems and How to Prevent Them
Tube feeding has come a long way since it was first invented. Modern PEG tubes are discreet, comfortable, and relatively easy to maintain. Still, complications can arise. That’s why it’s so important for family caregivers to know how to spot common PEG tube problems.
Read More >
Chad Birt is a freelance medical writer who resides in Astoria, Oregon. When he isn't behind a keyboard, you can find him hiking, camping, or birdwatching with his wife Ella and their two dogs, Diane and Thoreau.